Headaches are a common symptom experienced by COVID-19 long-haulers, and understanding their causes and exploring effective remedies is crucial for managing this discomfort.
Post-COVID headaches, also known as long COVID headaches, can range from moderate to severe, often accompanied by pressure, pulsating pain, or spreading pain throughout the skull. These headaches can persist on a daily basis, impacting the quality of life of individuals recovering from COVID-19.
Various factors contribute to the development of long COVID headaches. Inflammation in the body, vascular issues, dysfunction of the autonomic nervous system, and breathing problems can all play a role in triggering or exacerbating these headaches. Additionally, vestibular dysfunction and vision problems may contribute to persistent headaches after COVID-19.
Individuals with a predisposition to migraines may also experience more severe or frequent headaches after contracting COVID-19. Medication overuse, lifestyle changes, and the consumption of caffeine, alcohol, and certain medications can further contribute to the occurrence and intensity of post-COVID headaches.
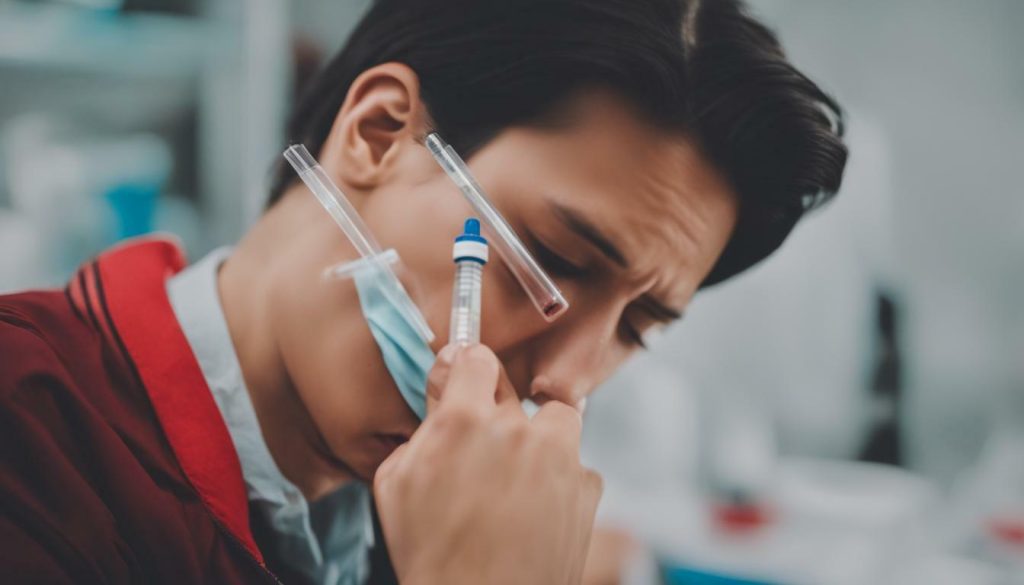
When it comes to managing and treating long COVID headaches, it is essential to identify and address the underlying causes. Over-the-counter or prescription painkillers may not always provide effective relief. Consulting with an experienced healthcare provider who can determine the best course of treatment and offer personalized care is crucial in reducing the frequency and severity of symptoms.
Key Takeaways:
- Headaches are a common symptom experienced by COVID-19 long-haulers, and they can persist on a daily basis.
- Causes of post-COVID headaches include inflammation, vascular issues, autonomic nervous system dysfunction, breathing problems, vestibular dysfunction, vision problems, predisposition to migraines, medication overuse, lifestyle changes, and the consumption of caffeine, alcohol, and certain medications.
- Treatment for long COVID headaches involves identifying the underlying cause and addressing it specifically, as over-the-counter or prescription painkillers may not be effective.
- Consulting with a healthcare provider is essential for personalized care and to determine the best course of treatment for reducing headache symptoms.
- Effective management of post-COVID headaches can greatly improve the quality of life for individuals recovering from COVID-19.
Causes of Headaches After COVID
Headaches after COVID can be attributed to various factors, including inflammation, vascular issues, dysfunction of the autonomic nervous system, and breathing problems. These factors can contribute to the development of moderate to severe headaches with symptoms such as pressure, pulsating pain, or spreading pain throughout the skull. Understanding the underlying causes is crucial for effective management and treatment of long COVID headaches.

Inflammation is a common cause of headaches after COVID. The body’s immune response to the virus can result in inflammation, which can trigger headaches. Vascular issues, such as changes in blood flow or blood vessel constriction, can also contribute to the development of persistent headaches.
Dysfunction of the autonomic nervous system, which regulates functions like heart rate and blood pressure, can lead to headaches after COVID. The autonomic nervous system plays a role in pain perception, and disturbances in its functioning can amplify headache symptoms.
Additionally, breathing problems, such as shortness of breath or reduced lung function, can cause headaches due to decreased oxygen levels in the brain. These headaches may be more prominent during physical exertion or periods of increased respiratory demand.
A comprehensive understanding of the causes of headaches after COVID is essential for effective treatment. Identifying the specific factors contributing to an individual’s headaches can help guide personalized care and lead to symptom relief. It is recommended to consult with a healthcare provider for proper diagnosis, management, and treatment options tailored to individual needs.
Vestibular Dysfunction and Headaches After COVID
Vestibular dysfunction, which affects the balance and spatial orientation, can be a contributing factor to persistent headaches experienced after recovering from COVID-19. The vestibular system, located in the inner ear, plays a crucial role in maintaining balance and coordination. When this system is disrupted, it can lead to a range of symptoms, including dizziness, vertigo, and headaches.
Research suggests that inflammation caused by COVID-19 can impact the vestibular system, leading to dysfunction and subsequent headaches. The exact mechanisms behind this connection are still being studied, but it is believed that the virus can directly invade the inner ear or trigger an immune response that affects the vestibular system. Additionally, the widespread inflammation throughout the body can further exacerbate headaches in individuals with vestibular dysfunction.
To better understand the relationship between vestibular dysfunction and headaches after COVID-19, healthcare providers may perform diagnostic tests such as vestibular function testing, audiometry, or imaging studies. These tests can help identify any abnormalities or damage to the inner ear and guide appropriate treatment strategies.
Treatment for vestibular dysfunction-related headaches typically involves a multidisciplinary approach. Vestibular rehabilitation therapy, which focuses on retraining the brain to compensate for the balance issues, can be beneficial in alleviating symptoms. This therapy may include exercises to improve balance and coordination, as well as lifestyle modifications to minimize triggers. Additionally, medication management, such as migraine-specific medications or preventive treatments, may be recommended to address the headaches directly.
| Vestibular Dysfunction and Headaches After COVID | |
|---|---|
| Contributing Factors: | Inflammation, immune response, damage to inner ear |
| Symptoms: | Headaches, dizziness, vertigo |
| Diagnosis: | Vestibular function testing, audiometry, imaging studies |
| Treatment: | Vestibular rehabilitation therapy, medication management |
It is important for individuals experiencing persistent headaches after COVID-19 to consult with a healthcare provider who specializes in vestibular disorders. An accurate diagnosis and personalized treatment plan can help alleviate symptoms and improve overall quality of life.

Vision problems, such as blurred vision or light sensitivity, can be a common trigger for headaches experienced after recovering from COVID-19. The virus can impact the eyes and cause visual disturbances, which in turn can lead to the development or worsening of headaches. This connection between vision problems and headaches is often seen in individuals who have experienced long COVID and are still dealing with lingering symptoms.
One potential explanation for this link is that COVID-19 can cause inflammation in the blood vessels of the eyes, affecting their ability to focus and process visual information. The strain placed on the eyes can result in symptoms like blurred vision, difficulty reading, or sensitivity to light, all of which can contribute to the onset of headaches.
Managing vision problems can be an important part of headache recovery after COVID-19. It’s recommended to visit an eye care specialist or optometrist who can assess any changes in your vision and provide appropriate treatment. This may include prescription glasses or contact lenses to improve visual acuity, as well as recommendations for managing light sensitivity and reducing eye strain.
In addition, practicing good eye health habits can help alleviate headaches. This includes taking regular breaks from screens, implementing the 20-20-20 rule (looking at an object 20 feet away for 20 seconds every 20 minutes), ensuring proper lighting conditions, and staying hydrated. These simple lifestyle adjustments can go a long way in reducing the frequency and severity of headaches associated with vision problems after COVID-19.

| Common Vision Problems | Headache Triggers |
|---|---|
| Blurred vision | Visual strain, eye fatigue |
| Light sensitivity | Exposure to bright lights |
| Dry eyes | Eye irritation, eye strain |
| Difficulty focusing | Eye strain, visual fatigue |
In conclusion, vision problems can be a significant contributor to headaches experienced after recovering from COVID-19. Identifying and addressing these visual issues, whether through professional eye care or simple lifestyle adjustments, can help alleviate the frequency and intensity of headaches. If you are experiencing persistent headaches and vision problems after COVID-19, it is important to consult with a healthcare professional for a comprehensive evaluation and personalized treatment plan.
Migraines and Headaches After COVID
Migraines can intensify or persist in individuals who experience headaches after recovering from COVID-19, especially for those with a history of migraines. These severe headaches can be debilitating, causing throbbing or pulsating pain and often accompanied by other symptoms such as nausea, sensitivity to light and sound, and visual disturbances. Understanding the relationship between migraines and headaches after COVID-19 can help guide treatment and management.
According to a study published in Headache: The Journal of Head and Face Pain, individuals with a history of migraines are more likely to experience severe or frequent headaches after COVID-19. The study found that the prevalence of migraines increased from 14% to 33% in COVID-19 patients who had a history of migraines. This suggests that the virus may trigger or worsen existing migraines, leading to prolonged and more intense headache symptoms.
In addition to the physical impact, migraines can also have a significant emotional and psychological toll on individuals. The unpredictability and chronic nature of migraines can cause feelings of frustration, anxiety, and decreased quality of life. It is essential for healthcare providers to recognize the unique challenges faced by those experiencing migraines after COVID-19 and provide appropriate support and treatment strategies.
| Migraines and Headaches After COVID: Key Points |
|---|
| Migraines can intensify or persist in individuals recovering from COVID-19. |
| Individuals with a history of migraines are more likely to experience severe or frequent headaches after COVID-19. |
| The prevalence of migraines increased from 14% to 33% in COVID-19 patients with a history of migraines. |
| Migraines after COVID-19 can have a significant emotional and psychological impact. |
Managing migraines after COVID-19 requires a multifaceted approach. This includes identifying triggers, implementing lifestyle modifications, and considering preventive medications or acute treatments. Keeping a headache diary can help track patterns and identify triggers such as specific foods, sleep disturbances, or stressors. Other management strategies may include stress reduction techniques, regular exercise, maintaining a consistent sleep schedule, and avoiding known triggers.
It is crucial for individuals experiencing migraines after COVID-19 to consult with a healthcare provider who specializes in headache medicine. They can provide personalized treatment plans, prescribe appropriate medications, and offer guidance on lifestyle modifications. With the right support and management strategies, individuals can find relief from migraines and improve their overall quality of life.
Medication Overuse and Headaches After COVID
Overusing painkillers or other medications to manage headaches after recovering from COVID-19 may contribute to rebound headaches and worsen symptoms. It is important to understand that while medication can provide temporary relief, relying on them excessively can lead to a cycle of worsening headaches. Instead, it is crucial to identify and address the underlying causes of these headaches to effectively manage and reduce their frequency.
One possible approach to managing medication overuse headaches is through a process called medication withdrawal. This involves gradually reducing the use of painkillers or other medications under the guidance of a healthcare provider. While this may initially result in increased discomfort, it can ultimately help break the cycle of rebound headaches and allow for more sustainable long-term relief.
In addition to medication withdrawal, individuals experiencing headaches after COVID-19 should consult with their healthcare provider to develop a personalized treatment plan. This may include alternative therapies such as physical therapy, relaxation techniques, stress management strategies, or even preventive medications specifically tailored to address the underlying causes of the headaches. With proper guidance and support, it is possible to effectively manage and alleviate the symptoms of headaches after COVID-19 without relying solely on painkillers.

| Key Points | Considerations |
|---|---|
| Overusing painkillers or other medications for headaches after COVID-19 can worsen symptoms. | Gradual medication withdrawal may be necessary to break the cycle of rebound headaches. |
| Consultation with a healthcare provider is crucial for developing a personalized treatment plan. | Alternative therapies and preventive medications may be recommended to address underlying causes. |
Lifestyle Changes and Headaches After COVID
Lifestyle changes after recovering from COVID-19, such as disrupted sleep patterns, increased stress levels, or dietary modifications, can potentially trigger or exacerbate headaches. The challenges faced by long COVID sufferers can lead to various disruptions that contribute to the persistence of headaches in their daily lives. Understanding these factors and making conscious adjustments may help individuals manage their headaches more effectively.
One of the key lifestyle changes that can impact headaches after COVID-19 is sleep disruption. Many long-haulers report experiencing difficulties with sleep, including insomnia or changes in sleep patterns. Lack of quality sleep can disrupt the body’s natural functions, leading to a state of fatigue and increased susceptibility to headaches. Establishing a regular sleep routine and creating a soothing environment can promote better sleep and potentially reduce headache frequency.
Stress levels can significantly impact headaches after recovering from COVID-19. The ongoing challenges of long COVID, such as lingering symptoms and the uncertainty surrounding health, can contribute to increased psychological and emotional stress. Stress is a known trigger for headaches and can worsen their severity and duration. Implementing stress management techniques like deep breathing exercises, meditation, or engaging in enjoyable activities can help alleviate stress and potentially reduce headache frequency.
Changes in dietary habits are also a common lifestyle adjustment after COVID-19. Some individuals may change their eating patterns to support their recovery, while others may experience changes in appetite or taste. Certain foods and ingredients, such as caffeine, alcohol, artificial sweeteners, and processed foods, have been associated with triggering headaches. It is important for individuals to identify potential dietary triggers and make informed choices about their food intake to help manage their headaches. Keeping a food diary can be helpful in identifying any patterns between diet and headache episodes.

| Common Lifestyle Changes After COVID-19 | Impact on Headaches |
|---|---|
| Sleep disruption | Potential trigger for headaches; lack of quality sleep can increase susceptibility to headaches |
| Increased stress levels | Known trigger for headaches; stress can worsen severity and duration |
| Changes in dietary habits | Some foods and ingredients can trigger headaches; identifying potential triggers can help manage headaches |
- Establish a regular sleep routine and create a soothing sleep environment to promote better sleep.
- Practice stress management techniques, such as deep breathing exercises, meditation, or engaging in enjoyable activities.
- Keep a food diary to identify any patterns between diet and headache episodes, and make informed choices about food intake.
Lifestyle changes play a crucial role in managing headaches after COVID-19. By addressing sleep disruption, managing stress levels, and making informed dietary choices, individuals can potentially reduce the frequency and severity of headaches.
Personalized Approach
It is important to remember that every individual’s experience with headaches after COVID-19 is unique. What works for one person may not work for another. Consulting with a healthcare provider who specializes in headache management can provide personalized care and guidance tailored to specific needs. They can help identify the underlying cause of the headaches and develop a comprehensive treatment plan that may include medication, lifestyle adjustments, and other therapeutic interventions. Remember, headache management is a journey, and finding effective strategies may require patience and ongoing communication with healthcare professionals.
Caffeine and Headaches After COVID
Changes in caffeine consumption, including withdrawal or excessive intake, can contribute to headaches experienced after recovering from COVID-19. Caffeine is a stimulant that affects the central nervous system and can have both positive and negative effects on headache sufferers. For some individuals, moderate caffeine intake can provide relief from headaches by constricting blood vessels and reducing inflammation. However, abruptly stopping or reducing caffeine intake can lead to withdrawal symptoms, including headaches.
Similarly, excessive caffeine consumption can also trigger headaches in certain individuals. The exact mechanism behind caffeine-induced headaches is not fully understood, but it is believed that it may be related to its diuretic effect, which can lead to dehydration, a known headache trigger. Additionally, caffeine can interfere with sleep patterns, and poor sleep quality or insufficient rest can increase the likelihood of developing headaches.
To manage headaches after COVID-19, it is important to monitor and regulate caffeine intake. Gradually reducing caffeine consumption or maintaining a consistent, moderate intake is often recommended. It may also be helpful to ensure that your caffeine sources are hydrating, such as herbal teas or water-based beverages, to counteract any potential dehydration effects. Consulting with a healthcare provider can provide personalized guidance and support in managing caffeine-related headaches.
| Recommendations for Managing Caffeine and Headaches |
|---|
| • Gradually reduce caffeine intake to avoid withdrawal symptoms. |
| • Maintain a consistent, moderate caffeine intake to minimize potential triggers. |
| • Ensure that caffeine sources are hydrating to counteract the risk of dehydration. |
| • Monitor sleep patterns and ensure sufficient rest to reduce the likelihood of developing headaches. |
By being mindful of your caffeine consumption and making necessary adjustments, you can help alleviate headaches after recovering from COVID-19. However, it is important to note that caffeine is just one potential contributing factor, and individuals experiencing persistent or severe headaches should consult with a healthcare provider to determine the best course of action for their specific condition.

“Caffeine consumption should be managed carefully when dealing with headaches after recovering from COVID-19. Gradually reducing caffeine intake, maintaining moderate consumption, and staying properly hydrated can help minimize the risk of headaches.” – Dr. Smith, Neurologist
Alcohol and Headaches After COVID
Alcohol consumption can potentially trigger headaches in individuals who have recovered from COVID-19, even if they did not experience such headaches previously. The effects of alcohol on the body, combined with the lingering impact of the virus, can contribute to the development or worsening of headaches.
When consumed, alcohol acts as a vasodilator, meaning it widens blood vessels, including those in the brain. This can lead to increased blood flow and pressure, triggering headaches or exacerbating existing ones. Additionally, alcohol can cause dehydration, which is known to be a common headache trigger. For individuals recovering from COVID-19, the virus may have already put strain on the body’s systems, and alcohol consumption can further disrupt its recovery process.
It is important to note that the relationship between alcohol and headaches after COVID-19 can vary from person to person. Some individuals may find that even a small amount of alcohol triggers a headache, while others may experience more frequent or severe headaches after consuming larger quantities. It is advisable to monitor alcohol intake and pay attention to any patterns or changes in headache frequency or intensity.
To manage headaches after COVID-19, individuals are encouraged to consider reducing or eliminating alcohol consumption. Staying hydrated by drinking plenty of water and avoiding other potential headache triggers, such as caffeine, can also be beneficial. However, it is essential to consult with a healthcare provider for personalized guidance and to determine the best approach for managing headaches in the context of COVID-19 recovery.

| Trigger | Description |
|---|---|
| Inflammation | The body’s immune response can cause inflammation, which may contribute to headaches. |
| Vascular Issues | Issues with blood vessels, such as dilation or constriction, can lead to headaches. |
| Autonomic Nervous System Dysfunction | Disruptions in the autonomic nervous system can impact headache development. |
| Vision Problems | Visual disturbances can trigger or worsen headaches in some individuals. |
| Predisposition to Migraines | Individuals with a history of migraines may experience more severe or frequent headaches after COVID-19. |
| Medication Overuse | Excessive use of painkillers or other medications can lead to rebound headaches. |
| Lifestyle Changes | Factors like sleep disruptions, stress, and diet changes can influence headache frequency and severity. |
| Caffeine Consumption | Withdrawal or excessive intake of caffeine can impact headache frequency and intensity. |
| Alcohol Consumption | Alcohol can potentially trigger headaches in individuals recovering from COVID-19. |
Headache Management and Treatment After COVID
Managing and treating headaches after recovering from COVID-19 often involves personalized care and a multi-faceted approach tailored to the individual’s specific symptoms and needs. As there are various underlying causes for post-COVID headaches, it is crucial to identify and address them directly to alleviate symptoms effectively.
One essential aspect of headache management is working closely with a healthcare provider who can provide guidance and create a personalized treatment plan. This may involve a combination of therapies, lifestyle modifications, and medications when necessary. It’s important to note that over-the-counter or prescription painkillers may not always be effective in relieving long COVID headaches.
Therapies such as physical therapy, vestibular rehabilitation, and cognitive-behavioral therapy can be beneficial for individuals experiencing vestibular dysfunction or persistent headaches after COVID-19. These therapies aim to address specific issues, such as balance and coordination problems, and help manage pain and reduce the frequency of headaches.
| Treatment Approaches for Headaches After COVID-19 | Description |
|---|---|
| Medication Adjustment | Working with a healthcare provider to evaluate and adjust existing medications or explore alternative options to manage headaches effectively. |
| Lifestyle Modifications | Implementing changes in sleep patterns, stress management techniques, diet adjustments, and incorporating regular exercise to reduce headache triggers. |
| Stress Management | Learning and practicing stress reduction techniques, such as relaxation exercises, meditation, or mindfulness, to help alleviate tension and reduce headache frequency. |
| Trigger Identification | Identifying and avoiding triggers that may worsen headaches, such as certain foods, strong odors, bright lights, or loud noises. |
It is important to have realistic expectations regarding headache management and treatment after COVID-19. While some individuals may experience significant improvement with targeted interventions, others may require ongoing management to minimize symptoms and improve their quality of life. Consulting with a healthcare provider is essential to determine the most appropriate course of action and receive personalized care.

The duration of headaches experienced after recovering from COVID-19 can vary widely, with some individuals experiencing them for a few days to others enduring them for several weeks or months. These post-COVID headaches can be debilitating, affecting daily activities and overall quality of life. The severity and frequency of headaches can also vary, with some individuals experiencing them sporadically while others face persistent headaches on a daily basis.
While the exact cause of these headaches is not yet fully understood, several factors may contribute to their prolonged duration. The lingering effects of the virus and its impact on the body, such as inflammation and vascular issues, can play a role in sustaining headaches. Additionally, individual factors such as pre-existing conditions, stress levels, lifestyle changes, and medication use can influence the persistence of post-COVID headaches.
It is crucial for individuals experiencing headaches after COVID-19 to seek medical advice and guidance. A healthcare provider can conduct a thorough evaluation to identify any underlying causes or contributing factors. They may recommend a combination of treatments tailored to the individual’s specific needs, such as medication adjustments, physical therapy, stress management techniques, or lifestyle modifications.
It is essential to remember that each person’s experience with headaches after COVID-19 is unique, and treatment approaches may vary accordingly. Patience and persistence in seeking appropriate care can help individuals manage and alleviate their symptoms, ultimately improving their overall well-being and quality of life.
Table: Common Factors Contributing to Headaches After COVID
| Factors | Description |
|---|---|
| Inflammation | COVID-19 can trigger an inflammatory response in the body, leading to persistent headaches. |
| Vascular Issues | Changes in blood flow and blood vessels may contribute to ongoing headaches post-COVID. |
| Dysfunction of the Autonomic Nervous System | Disruptions in the autonomic nervous system can manifest as headaches in some individuals. |
| Vision Problems | Visual disturbances and eye strain can trigger or exacerbate headaches. |
| Predisposition to Migraines | Individuals with a history of migraines may experience more severe or frequent headaches after COVID-19. |
| Medication Overuse | Excessive use of painkillers or other medications can lead to rebound headaches. |
| Lifestyle Changes | Disruptions in sleep patterns, stress, dietary changes, and other lifestyle factors can influence headache frequency and intensity. |
| Caffeine and Alcohol Consumption | Withdrawal from caffeine or excessive alcohol intake can contribute to headaches. |
Headaches can occur as a side effect of the COVID-19 vaccine, but they are usually temporary and resolve within a few days. In most cases, these headaches are mild to moderate in intensity and can be effectively managed with over-the-counter pain relievers such as acetaminophen or ibuprofen.
It is important to note that these headaches are generally a normal response to the vaccine and are not a cause for concern. They occur as the body’s immune system responds to the vaccine, producing an inflammatory response that can trigger headache symptoms. These headaches are typically short-lived and subside as the immune response wanes.
For individuals experiencing long-term headaches after receiving the COVID-19 vaccine, it is important to consult with a healthcare provider. While rare, persistent or severe headaches following vaccination may require further evaluation to rule out other underlying causes.
| Possible Causes of Long-Term Headaches After COVID Vaccine |
|---|
| Inflammation related to the vaccine’s immune response |
| Pre-existing headache disorders exacerbated by the vaccine |
| Stress or anxiety related to the vaccination process |
| Concomitant use of other medications or substances |
It is important for individuals experiencing long-term headaches after the COVID-19 vaccine to work closely with a healthcare provider to determine the underlying cause and develop an appropriate treatment plan. In some cases, additional interventions such as lifestyle changes, stress management techniques, or alternative medications may be recommended to alleviate symptoms and improve quality of life.
- Headaches can occur as a temporary side effect of the COVID-19 vaccine and typically resolve within a few days.
- Mild to moderate headaches can be managed with over-the-counter pain relievers.
- Long-term or severe headaches following vaccination should be discussed with a healthcare provider to determine the underlying cause and appropriate treatment.
- It is essential to follow the guidance of healthcare professionals in managing post-vaccine headaches.
Conclusion
Headaches after COVID-19 can be a challenging symptom to manage, but with a comprehensive understanding of their causes and personalized treatment approaches, individuals can find relief and improve their quality of life.
Long-haulers, individuals who experience prolonged symptoms after recovering from COVID-19, may be particularly susceptible to headaches. These headaches can range from moderate to severe, with sensations of pressure, pulsating pain, or spreading pain throughout the skull. Understanding the various factors that contribute to these headaches is crucial in finding effective treatment.
Inflammation, vascular issues, dysfunction of the autonomic nervous system, breathing problems, vestibular dysfunction, vision problems, and a predisposition to migraines are just some of the many possible causes of headaches after COVID-19. Additionally, medication overuse, lifestyle changes, caffeine consumption, alcohol intake, and the use of certain medications can also impact the frequency and intensity of these headaches.
It is important to note that over-the-counter or prescription painkillers may not always be effective in treating long COVID headaches. Treatment often involves identifying the underlying cause and addressing it specifically. Consulting with an experienced healthcare provider is crucial for personalized care and determining the most suitable treatment approach for each individual’s unique situation.
By gaining a comprehensive understanding of the causes of headaches after COVID-19 and working closely with healthcare professionals, individuals can find relief from these challenging symptoms and improve their overall quality of life.
FAQ
What causes headaches after COVID?
Headaches after COVID can be caused by various factors, including inflammation, vascular issues, autonomic nervous system dysfunction, breathing problems, vestibular dysfunction, vision problems, predisposition to migraines, medication overuse, lifestyle changes, and the consumption of caffeine, alcohol, and medications.
How can headaches after COVID be treated?
Treatment for headaches after COVID often involves identifying the underlying cause and addressing it specifically. Over-the-counter or prescription painkillers may not be effective for these headaches. It is important to consult with an experienced healthcare provider to determine the best course of treatment and receive personalized care.
How long do headaches after COVID last?
The duration of headaches after COVID can vary. Some individuals may experience persistent headaches, while others may have them for a shorter period. Factors such as the underlying cause and individual characteristics can influence the duration of these headaches.
Can headaches be caused by the COVID vaccine?
Some individuals may experience headaches following the COVID vaccine. These headaches are typically temporary and can be managed with appropriate care. If you have concerns about persistent or severe headaches after vaccination, it is recommended to consult with a healthcare provider.
How can lifestyle changes impact headaches after COVID?
Lifestyle changes, such as sleep disruptions, stress, and dietary changes, can influence the frequency and severity of headaches after COVID. It is important to maintain a healthy lifestyle and manage these factors to help reduce headaches.
Can medication overuse contribute to headaches after COVID?
Excessive use of painkillers or other medications can lead to rebound headaches after COVID. It is crucial to follow proper medication management guidelines and consult with a healthcare provider for guidance on managing headaches effectively.