If you have diabetes, taking good care of your feet is very important. Complications from diabetes can lead to things like foot ulcers. These could eventually mean you need an amputation. Knowing the 6 stages of a diabetic foot helps with both prevention and treatment.
Key Takeaways:
- Proper diabetic foot care is crucial in preventing severe complications.
- Diabetic neuropathy can lead to pain and discomfort in the foot.
- Superficial and deep ulcers can develop as the condition progresses.
- Ulcers reaching the bone and forefoot gangrene pose serious risks.
- Full-foot gangrene may require amputation if not treated promptly.
Stage 1: Pain In Foot

Identifying Stage 1 of a Diabetic Foot
Stage 1 of a Diabetic Foot shows pain in the foot. This pain comes from diabetic neuropathy. It’s a nerve problem often seen in people with diabetes. Symptoms can be a mix of tingling, burning, or sharp pains in the feet.
At the start, you might feel a bit uncomfortable or the feet might seem sensitive. Walking or standing for long can be hard, and the foot may feel different in temperature or sensation. It’s crucial to notice these early signs. Getting help early can stop the problem from getting worse.
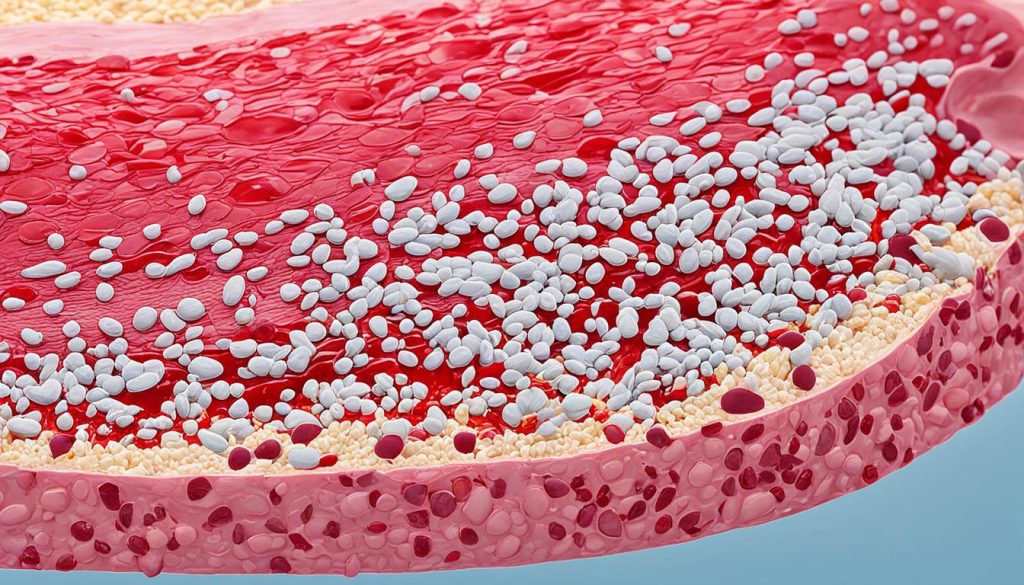
Stage 2: Superficial Ulcer
Stage 2 of a Diabetic Foot might cause a superficial ulcer. This is an open sore found in weight-bearing areas of the feet. It’s not as deep as some ulcers and can be cared for with good foot hygiene.
It’s vital to keep the ulcer clean to prevent infection and aid healing. Wash the area gently with mild soap and water to clear it of debris. Dry the ulcer well with a clean towel or sterile pad to avoid too much moisture.
Choosing the right dressing for the ulcer is key to its care. The best type of dressing varies based on the ulcer’s depth, how big it is, and the wound’s condition. Your healthcare provider can advise on the best dressing.
Reducing pressure on the affected area also helps with healing. This is done by wearing special shoes or adding inserts for pressure relief. Sometimes, a doctor might suggest using a cast or a walking boot.
Good wound care and keeping your feet clean are the best ways to handle a Stage 2 ulcer. Always check in with your healthcare team and act fast if you notice changes. They can guide you to ensure your wound heals well.
Stage 3: Deep Ulcer
In Stage 3 of a Diabetic Foot, a deep ulcer forms, reaching down into the skin and tissues beneath. Quick, effective treatment is key now. It stops more problems and helps the wound heal.
For a Stage 3 ulcer, wound debridement is a usual step in treatment. This means taking out dead or bad tissue from the wound area. It lets the healthy tissue grow and speeds up healing. Wound debridement also lowers infection risk and makes the wound healthier.
Ensuring treatment is crucial as infections are a big risk at this stage. Treating with antibiotics may be needed. This step fights off the infection and keeps it from spreading.
To fully manage a Stage 3 ulcer, looking at its main causes is important. Things like nerve problems and blood flow issues. A good diabetic foot care plan can stop the ulcer from getting worse. It also helps heal it better and avoids more problems.
| Stage 3: Deep Ulcer | Symptoms | Treatment |
|---|---|---|
| Penetration of deeper layers of skin and tissues | – Visible deep ulcer – Pain and tenderness at the ulcer site – Foul odor or discharge from the wound |
– Wound debridement to remove dead or infected tissue – Antibiotic treatment to control infections – Offloading pressure from the ulcer area – Managing underlying causes like neuropathy and vascular insufficiency |
Stage 4: Ulcer Reaches Bone

Spotting Stage 4 of a Diabetic Foot is key to stop more issues and get right treatment. This stage means the ulcer is into the bone, leading to osteomyelitis, a bone infection. It’s hard to treat and needs strong efforts.
Surgery to clean out dead or bad tissue is usually needed to help heal. Taking antibiotics is crucial to beat the infection. It’s also important to keep an eye on the ulcer and take great care of the wound and foot overall.
Working closely with experts like podiatrists or wound care doctors is vital to make a good treatment plan. They guide you on using antibiotics right, picking the best wound dressings, and ways to lessen pressure on the ulcer.
| Infection Treatment Options for Stage 4 of a Diabetic Foot |
|---|
| Surgical debridement |
| Antibiotic therapy |
| Regular monitoring |
| Proper wound care |
| Offloading techniques |
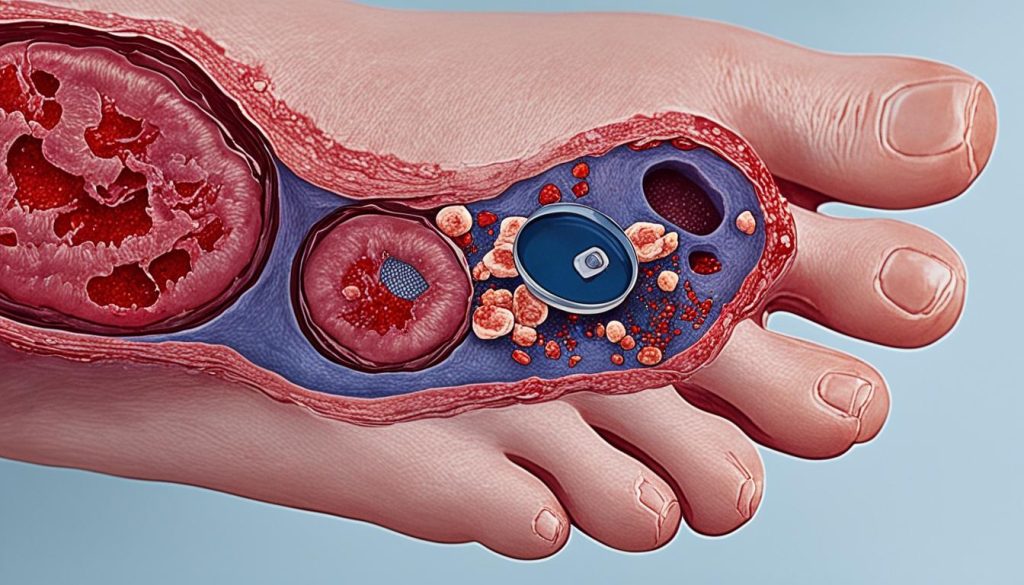
Stage 5: Forefoot Gangrene
In Stage 5, a Diabetic Foot has forefoot gangrene. This happens when the front foot tissue dies from lack of blood. It’s a serious issue, possibly leading to amputation if not treated fast.
Detecting Stage 5 involves careful watch, checking blood flow, and talking to doctors. Acting early is key to stop the gangrene from getting worse and lower the amputation risk.
Forefoot gangrene is a dire effect of diabetic foot issues. Blood vessels squeezing too much can stop vital blood flow. This lack of blood kills the tissue, causing gangrene.
Keeping a close eye, assessing well, and teaming up with health experts like podiatrists matter a lot in this case. Fast actions, such as surgery to improve blood flow and using antibiotics, can save the foot from getting amputated.
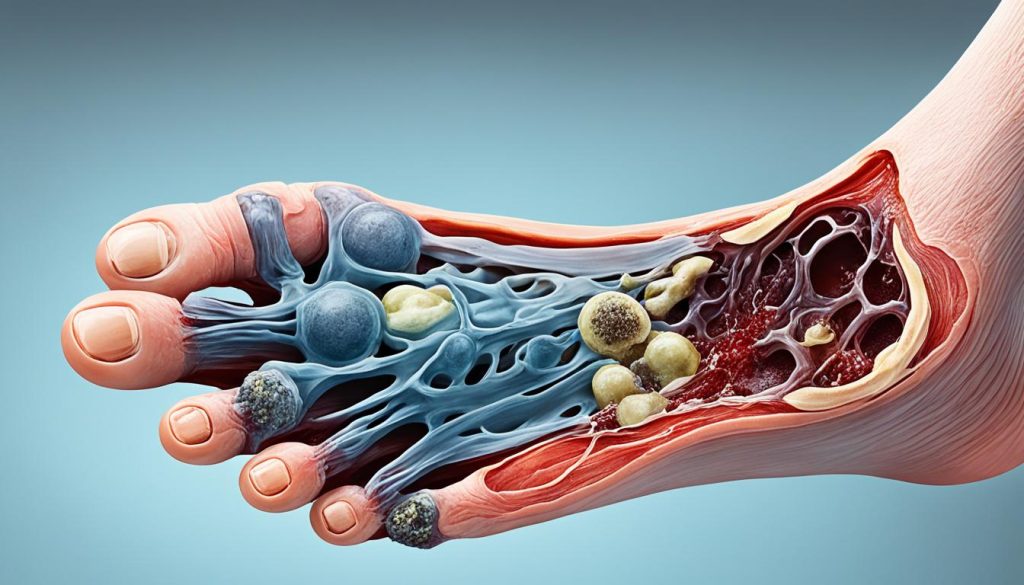
Stage 6: Full-Foot Gangrene
Full-Foot Gangrene is the most advanced stage of a Diabetic Foot. It happens when the whole foot is damaged by gangrene. This condition can be life-threatening and may require an amputation.
Acting early and treating the condition aggressively are key to avoid this severe stage. So, it’s vital to identify signs and symptoms sooner.
Keeping your feet cared for, working closely with healthcare providers, and managing diabetes well can help prevent Full-Foot Gangrene.
Conclusion
Proper diabetic foot care is key in stopping and reducing the problems linked to the 6 Stages of a Diabetic Foot. By spotting early signs and acting early, like keeping blood sugar in check and keeping feet clean, those with diabetes can cut the risk of serious foot issues. This also helps make their foot health better overall.
It’s crucial to keep a close eye on foot health. You should look out for any pain, discomfort, or ulcers. Also, check foot temperature and feeling. It’s vital to work closely with pros like podiatrists or diabetes experts. They help manage each stage of the diabetic foot and make a treatment plan that’s just right for you.
Good wound care is a must to stop more issues and help wounds heal. This means cleaning and dressing ulcers or wounds and lessening pressure on them. It’s also important to treat underlying problems like nerve issues or poor blood flow. This tackles the real reasons for the diabetic foot and stops it from getting worse.
Making diabetic foot care a top priority helps prevent problems. This lets people with diabetes keep their foot health safe and improves their life quality. The key is to always be on the lookout, keep learning, and work closely with healthcare providers to handle the different stages of a diabetic foot.




